Screening
Health screening is a well-established strategy to promote early detection of illness in at risk groups. Screening for common psychiatric disorders, such as PTSD, can significantly improve rates of diagnosis and reduce time to appropriate treatment, thus overall improving outcomes. Considering the risk for repeated traumatic exposures with First Responders, screening for signs of psychological injury is strongly supported. Those at risk for suicide and other serious mental disorders would also benefit from early and sometimes urgent intervention.
Mental health screening should be offered to all staff in all sectors who may be suffering from a mental health illness including PTSD. Screening should be available for all staff, who have been exposed to traumatic incidents and may be suffering from work-related PTSD.
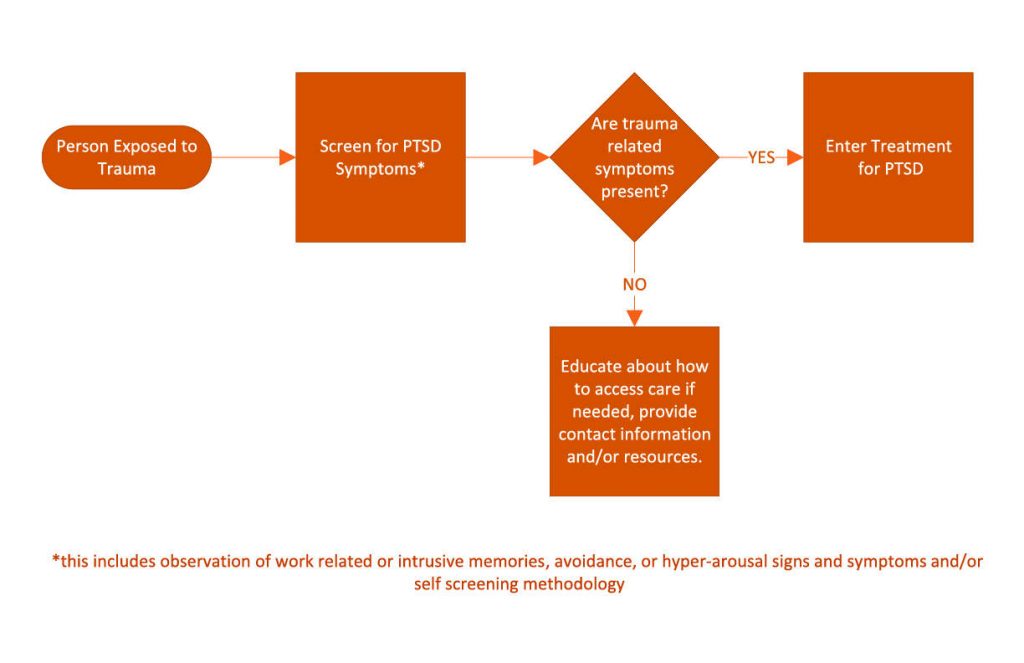
The following protocol is recommended for employers and occupational health departments:
- Identify employees that have been exposed to serious incidents, a repeated number of events or who are distressed as a result of any traumatic incident.
- Once identified, occupational health or other trained staff can deliver by phone or in-person, a screening instrument or protocol.
- This would serve to identify symptomatic individuals early in the course of and those who develop progressive symptoms of PTSD.
- Those individuals who screen positive based on a fixed cut-off score would be referred for further assessment and treatment if indicated.
- Screening should be conducted within 1 month and at 3 and 6 months after serious or repeated exposures.
A positive response to a screen does not necessarily indicate that an employee has Posttraumatic Stress Disorder. However, a positive response does indicate that an employee may have PTSD or trauma-related problems and further investigation of trauma symptoms by a mental-health professional may be warranted.
Specifically for PTSD, several screening methods have been developed. In general, a good screening instrument for PTSD would be brief, sensitive and reliable, consistently identifying those with potential symptoms. Screening tools are not intended to provide a diagnosis, but will help identify those who may require further assessment.
Screening models such as online mental health screening, in-depth mental health screening or routine mental health “check-ups”, or Primary Care (PC-PTSD) screening may be used. The screens do not include a list of potentially traumatic events, which should be tracked, conducted, and maintained by your organization’s Occupational Health and Safety Department.
Occupational Health professionals should be aware of and have access to validated screening tools for PTSD and other mental disorders. They should be trained in how to identify those at increased risk for PTSD, suicide and other mental disorders and refer to appropriate mental health professionals in a timely manner.
The Screening Program should also be re-evaluated annually by Occupational Health professionals and your JHSC to ensure screening is being consistently performed and those screening positive are seeking assessment and treatment.